Diabetes - Understanding the disease, types of treatments and the connection to pressure sores
Diabetes, treatment options and the connection to pressure ulcers
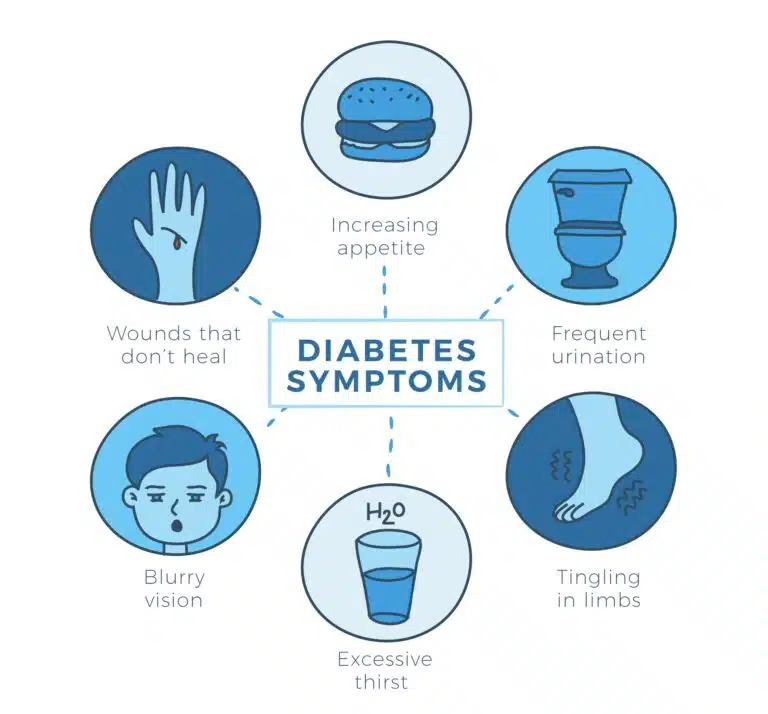
Diabetes is a chronic metabolic disorder that is considered one of the most common diseases in the world. The disease is divided into three main types: type 1 diabetes, type 2 diabetes, and gestational diabetes. Treatment of the disease combines drug, nutritional, and physical fitness approaches, each of which is designed to maintain normal blood glucose levels. In addition, diabetes makes it difficult for wounds to heal and increases the risk of pressure ulcers, which are wounds that form as a result of prolonged pressure on certain areas of the body. Pressure ulcers can develop on the legs, back, buttocks, and feet, and are divided into grades 1 to 4 depending on their depth and severity.
Types of diabetes
Type 1 diabetes
Type 1 diabetes is a chronic disease in which the pancreas, the organ that produces insulin in the body, fails to produce enough of the hormone. Insulin is needed to move sugar (glucose) from the blood into the body’s cells, where it is used as a source of energy. Without enough insulin, glucose builds up in the blood, causing high blood sugar levels and can lead to many medical conditions and diseases.
Type 1 diabetes usually develops in childhood or adolescence, but it can also occur in adults. Treatment for type 1 diabetes involves frequent blood sugar testing and daily insulin injections, either by self-administering insulin or by using an insulin pump. Treatment also emphasizes a balanced diet and exercise. The goal of these treatment approaches is to keep blood glucose levels within a normal range so that the progression of the disease and its side effects can be prevented or slowed.
It is important to note that because type 1 diabetes is a chronic disease, long-term medical management is required. Proper management of the disease can go a long way in maintaining the patient’s quality of life. In addition, there are many researchers trying to find new treatments and options for preventing type 1 diabetes. Patients and their families are advised to stay in close contact with their medical team and ask them any questions or concerns.
Type 2 diabetes
Type 2 diabetes is the most common type of diabetes and is characterized by resistance to or impaired production of insulin. Insulin is an essential hormone that allows glucose to enter cells and be used as a source of energy. In type 2 diabetes, the body cannot use insulin effectively, or the pancreas does not produce enough insulin, which causes high blood sugar levels.
The risk of developing type 2 diabetes increases with age, weight, physical inactivity, and a family history of diabetes. Treatment for type 2 diabetes includes the use of blood sugar-lowering medications, dietary changes, and an exercise program. The goal of treatment is to keep blood glucose levels within a normal range and to prevent or slow the progression of the disease and other health problems.
In addition, type 2 diabetes can cause pressure ulcers, especially on the feet. Pressure ulcers are wounds that result from prolonged pressure on certain areas of the body and can be especially dangerous in diabetic patients due to the high risk of the wounds worsening and spreading. Preventing and treating pressure ulcers is a significant part of managing the disease in diabetic patients.
Gestational diabetes
Gestational diabetes is a condition in which blood glucose levels are higher than normal during pregnancy. It may develop due to the effects of pregnancy hormones that reduce the body’s sensitivity to insulin. Gestational diabetes is usually detected during regular prenatal checkups and disappears after delivery. However, it increases the woman’s risk of developing type 2 diabetes later in life.
Treatment for gestational diabetes includes frequent blood glucose testing, a balanced diet, and exercise. Sometimes, insulin therapy will also be given. The goal is to maintain normal blood sugar levels to prevent harm to the fetus and mother.
Gestational diabetes can lead to increased fetal growth, which may cause difficulties during delivery and the need for a cesarean section. Children born to mothers with gestational diabetes may also be at higher risk of obesity and diabetes later in life. Because this condition is so common, screening for gestational diabetes is important to ensure proper medical management and prevent future risks to the mother and fetus.
Types of treatments
Drug treatment
Drug treatment of diabetes is critical to maintaining normal blood glucose levels. In type 1 diabetes, treatment involves daily injections of insulin or the use of an insulin pump. In type 2 diabetes, oral medications or insulin may be needed depending on how well blood glucose levels are controlled. In addition, there are medications that help improve the body’s sensitivity to insulin or slow down the stabilization of glucose in the liver.
Nutritional therapy
A balanced diet is an integral part of diabetes treatment. It is important to understand the impact of different foods on blood sugar levels and adjust your diet accordingly. Nutritional counseling with a dietitian can help people with diabetes build a healthy, balanced diet that will help them maintain normal blood glucose levels.
fitness
Regular physical activity helps keep blood sugar levels within a healthy range, improve the body’s sensitivity to insulin, and ensure a healthy weight. Physical fitness can also improve strength and flexibility, thereby reducing the risk of cardiovascular disease. It is important to find a type of physical activity that is specifically suitable for the patient and make it part of the daily routine. Start with light training and gradually increase the amount and intensity of the activity, while maintaining the frequency of testing blood sugar levels before and after the activity.
What are pressure sores?
Pressure ulcers are sores that form when there is prolonged pressure on a specific area of the body, usually in areas where the skin is thin and close to the bone, such as the buttocks, feet, back, or legs. The prolonged pressure interferes with blood flow and causes tissue damage. In severe cases, the sores can reach the muscle or bone. Diabetics are at higher risk for pressure ulcers due to problems with blood flow and skin sensitivity.
Additionally, slow wound healing and low pain sensitivity make early detection and treatment difficult. Pressure ulcers are graded from 1 (initial wound) to 4 (deep wound to the bone). Proper blood glucose management, frequent skin examinations, and early wound treatment can help prevent pressure ulcers or minimize their spread.
Pressure sores on the legs
Pressure ulcers are a common problem among diabetics, mainly due to poor blood circulation and reduced sensitivity to pain. They form when there is prolonged pressure on certain areas of the foot, such as the heel or ball of the foot. The prolonged pressure can cause tissue damage and impaired blood flow, leading to ulcers. Diabetic patients may have reduced sensitivity in their feet, which makes them less aware of ulcers in the early stages.
The slow healing of wounds in diabetic patients makes it difficult to treat pressure ulcers. This can lead to the deterioration of the wounds and the need for additional and prolonged treatments. Prevention of pressure ulcers and their early detection are especially important for diabetic patients to prevent infections and further problems.
Pressure sores on the back
Pressure ulcers on the back are common among people who spend a lot of time in bed or in a wheelchair, and in general among patients with limited mobility. The prolonged pressure interferes with blood flow to the skin and underlying tissues, causing tissue damage and sores. The most common area for pressure ulcers on the back is the shoulder blades.
Depending on the person’s level of pain and sensitivity, they may not notice the wound in the early stages, so frequent examination and preventive measures are very important. Prevention of pressure sores on the back includes frequent breaks in pressure on the affected area as well as maintaining personal hygiene and frequent examination of the skin. Early treatment of pressure sores can prevent the progression of the wounds and help maintain the person’s quality of life.
Pressure sores on the buttocks
Pressure ulcers on the buttocks are caused by prolonged pressure on the buttocks, especially in people who spend a lot of time sitting or lying down. The prolonged pressure on the skin and tissues impairs blood flow and leads to tissue damage. Diabetic patients have low sensitivity, and together with poor blood flow, the risk of pressure ulcers increases and the rate of recovery from them slows down.
Preventing pressure sores on the buttocks includes regular physical activity and changing positions frequently to relieve pressure on the area. In addition, emphasis should be placed on hygiene and frequent skin examinations. Early treatment of pressure sores when they are in the early stages can help prevent the progression of the sores and maintain the patient’s quality of life. The chemistry between the doctor and the patient and the recommendations for preventing pressure sores on the buttocks can be a decisive factor in preventing and treating these sores.
Pressure sores on the foot
Pressure ulcers are common in people who are bedridden or wheelchair bound, especially in diabetics who have problems with blood flow and skin sensitivity. Prolonged pressure on certain areas of the foot, such as the heel or toes, can damage the tissues and cause tissue damage. These ulcers can develop into deep wounds if not treated promptly.
Additionally, diabetic patients may experience reduced sensation in their feet, which can make it difficult to identify the sores early. Prevention and early detection of pressure sores on the feet are especially important for diabetic patients, as they can promote healing and prevent infections and other problems. Exercise, frequent skin exams, thorough cleaning, and comfortable shoes are some of the measures to prevent and treat pressure sores on the feet.
Grades of pressure ulcers (from 1 to 4)
Grade 1 pressure sores
Grade 1 pressure ulcers are the first and mildest stage of pressure ulcers. The skin remains normal but there is widespread redness in the affected area that does not go away even after pressure is relieved on the foot. There may be a tingling or darkening in the area and it may be tender or warm to the touch. This stage requires early recognition and proper treatment to prevent progression to more severe stages.
Grade 2 pressure sores
At this stage, the skin fills up and an open wound is formed with damage to the upper or lower layer of skin. The wound can look like a burn or an area of pus. This is the stage where the wound may look like a fluid-filled blister or a relatively deep wound. Targeted treatment is important to prevent the damage from spreading.
Grade 3 pressure sores
At this stage, the damage expands and deepens towards the underlying muscle and fat. The wound is deep and reaches the muscle, but does not go through the muscle. It is possible that more extensive damage will be revealed than what is visible when the wound is opened. This stage requires immediate and professional medical treatment.
Grade 4 pressure sores
Grade 4 pressure ulcers are the most severe, with damage extending deep into the bone. The ulcers may cause loss of joints and damage to other tissues. Treatment at this stage requires immediate and professional medical intervention, and sometimes even surgery, to prevent the damage from spreading and further infections.
Preventing pressure ulcers in diabetic patients
It is important to note that the information provided here is for informational purposes only and does not constitute medical advice. A medical professional should be consulted before implementing any recommendation or action.
As part of the medical management of diabetic patients, the risk of pressure ulcers can also be addressed. Here are some steps that can reduce the risk of pressure ulcers in general and high-grade pressure ulcers in particular:
1. Daily skin check:
Daily skin examination in areas such as the buttocks, legs, and back may allow for early detection of potential changes and sores.
2. Maintaining personal cleanliness:
3. Matching shoes and clothes:
4. Frequent position changes:
5. Physical fitness:
6. Balanced diet:
7. Frequent medical checkups:
Regular visits to medical clinics specializing in pressure ulcer treatment can provide follow-up, expert recommendations, and personalized treatment. During these visits, skin tests can be performed to assess risk, receive recommendations for further treatment, or support in preventing pressure ulcers.
The most important recommendation is to consult a specialist who can provide a medical diagnosis personalized to your health condition.
Summary and continued learning: Coping with diabetes and pressure sores
Diabetes is a multifaceted disease that affects the quality of life of patients and requires dedicated medical management. During the article, we examined the types of diabetes: type 1 diabetes, type 2 diabetes, and gestational diabetes. We discussed the various treatment methods that include medication, nutrition, and maintaining physical fitness. Pressure ulcers are another problem that is important to pay attention to in the medical management of diabetic patients. We discussed their definition, their appearance in different areas of the body, and their severity. We emphasized the importance of preventing and early treating pressure ulcers, and we emphasized the importance of examinations at medical clinics specializing in the treatment of pressure ulcers. For additional and expanded information on each of the topics we discussed, it is recommended that you review additional pages on our website that offer more extensive information on diabetes and pressure ulcers. It is worth deepening your understanding and learning about additional ways to manage the disease and maintain skin health.
It is important to emphasize that the content presented in this article provides basic information and understanding about diabetes and pressure ulcers, and is not intended to replace professional medical advice. In any case of doubt or need, it is strongly recommended to consult a specialist physician in order to receive a medical diagnosis appropriate to your health condition.